iCAN

Fertility preservation and what to expect
There are many questions surrounding a cancer diagnosis, particularly when it comes to the subject of fertility.
Depending on factors such as diagnosis, treatment, fertility and age, the ability to conceive can be impacted by cancer treatment. Fertility preservation is an option for those looking to maintain their ability to conceive.
We spoke to Sydney gynaecologist Dr Rachael Rodgers, who specialises in fertility treatment and reproductive endocrinology. She explains what’s involved and why it’s crucial to have a conversation about fertility at diagnosis.
In many cases, something can be done to help preserve fertility before cancer treatment begins. Procedures including freezing eggs and ovarian tissue, along with ovary suppression injections, can help manage fertility in those undergoing chemotherapy. Even if the nature of the cancer or the urgency of treatment doesn’t allow us to preserve fertility, patients still have some options.
“In patients where we don’t have time to freeze eggs, we can give them monthly injections to suppress their ovaries and try to protect them as much as possible during chemo,” Dr Rodgers explains.
Dr Rodgers says she also offers support by monitoring the girls and explaining the cancer treatment phase as they go through it. Once treatment is finished, an assessment is provided to gauge their fertility and see what their options might be.
The other reason it can be valuable to seek fertility options because the psychological outcomes tend to be a lot better.
“Anecdotally speaking, though there’s a little bit of data to support it, to say that if you do everything you possibly can to preserve someone’s fertility before cancer treatment, but you don’t succeed, they come out the other end, and they’re at peace with what’s happened,” Dr Rodgers says.
She notes that patients who’ve tried all options but weren’t successful can tend to be more understanding and at peace with the outcome.
“Whereas if you don’t see a fertility specialist beforehand, then they come out the other end quite bitter saying well maybe it was possible, maybe I could have had children using my eggs, but nobody tried,” she notes.
What are my options?
Freezing eggs or embryos
The process of freezing eggs or embryos involves collecting, developing and storing eggs or embryos to allow for in-vitro fertilisation (IVF) at a later stage.
“Freezing eggs is the most reliable way of preserving fertility. Essentially, it’s ten days of hormone injections followed by an egg collection,” Dr Rodgers explains.
Freezing ovarian tissue
Ovarian tissue freezing is an experimental procedure for preserving fertility. The method involves removing one ovary and then separating the tissue containing your eggs from the rest of the ovary. This tissue is frozen and stored for use after cancer treatment, allowing for the possibility of a biological child.
“Some girls certainly pubertal girls and occasionally in other circumstances we can actually operate and take out some ovarian tissue and freeze it, with the plan being when they’re ready to have children later we can transplant back the ovarian tissue, and if it regrafts, then they can potentially ovulate and conceive naturally,” Dr Rodgers notes.
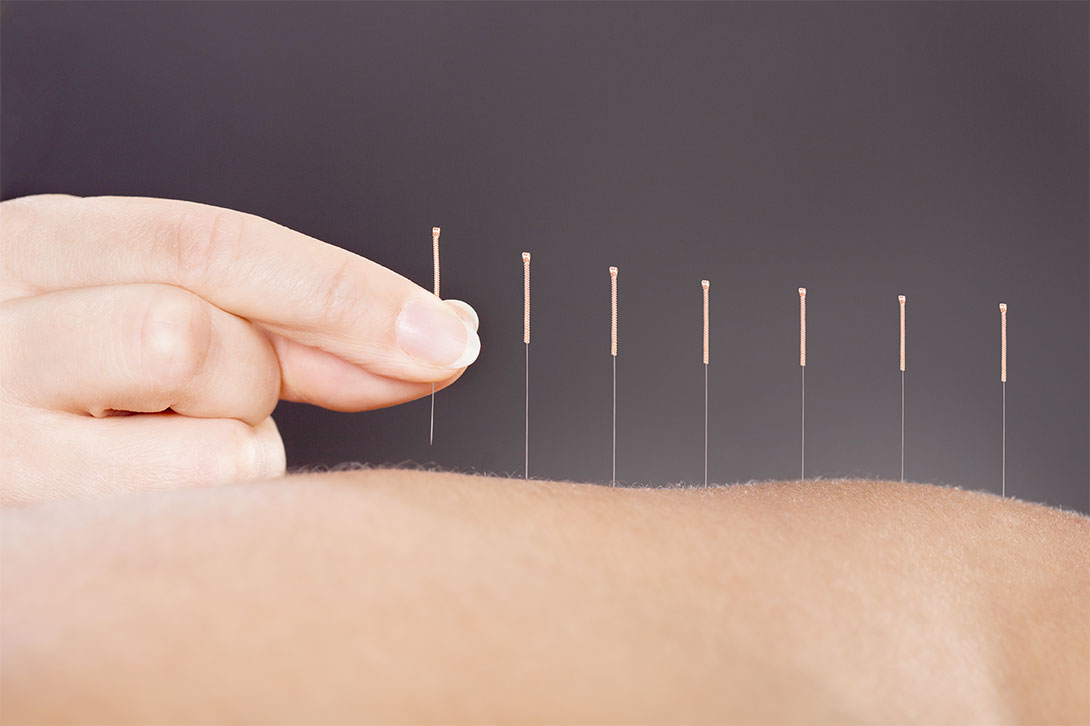
Ovary suppression injections
Also known as ovarian function suppression and ovarian ablation, ovarian suppression refers to the method of stopping the ovaries from making oestrogen.
Studies have shown that this suppression of the ovaries may protect them during chemotherapy as it temporarily deactivates the ovaries.
“The other thing we do is give patients hormone treatment that ‘down-regulates their ovaries during chemotherapy to protect the organs as much as possible. This treatment helps improve the chances that when they get their regular periods back, they can potentially conceive naturally,” Dr Rodgers says.
The myth of waiting for a period
Unlike the process of IVF, collecting eggs for fertility preservation can be done regardless of a person’s menstrual cycle.
“There’s a bit of a myth that the process must revolve around a woman’s period, but that’s not the case. With fertility preservation, it doesn’t matter when a patient’s period is due. One can start immediately collecting eggs for embryo cryopreservation (freezing),” Dr Rodgers explains.
“No matter what your cancer is or when you think (fertility) treatment needs to start, it’s always valuable to have an appointment with a fertility specialist immediately.”
The process
The process of freezing eggs involves ten days of hormone injections, followed by the harvesting of a woman’s eggs. The whole process lasts around twelve days, with Dr Rodgers noting that it’s relatively straightforward.
To begin, the fertility doctor does an initial assessment of the patient. At this time, a second appointment is made with the nursing staff to teach how to administer the daily hormone injections.
“We can often start hormone injections within 24 hours,” Dr Rodgers notes.
A week later, a series of follow-up appointments will determine when follicles are at the right size, which indicates when eggs are ready to be collected.
“The period of time from when they see the fertility specialist to the time that their eggs are collected is only about 12-14 days. So it’s really quite fast,” she says.
The egg collection procedure is conducted under a light general anaesthetic and takes up to half an hour.
Dr Rodgers notes it’s ideal if the patient is able to wait a minimum of five to seven days after egg collection before chemotherapy begins.
An emotional time
While the process might be quick, Dr Rodgers says it’s also a very emotional time for most women.
“Yes, it can be a very emotional couple of weeks. I work with fantastic nurses, and they are very good at supporting women through the journey. Many women come out the other end feeling at peace, knowing we’ve frozen their eggs. But there’s also the fact that we’ve been with them so closely through those two weeks and the patients get very bonded to everyone involved,” Dr Rodgers says.
Some female patients will likely go through menopause early. Dr Rodgers says, however, that both the symptoms and the implications of early menopause can be managed. With regards to future children, a number of eggs can be kept frozen. Patients can try for one baby and then further children down the line if they wish.
One woman’s experience
As for the actual process, Jess Braude, diagnosed with triple-negative breast cancer three years ago, has outlined what she went through during fertility preservation which has enabled her to undertake IVF successfully.
“The process began with daily injections of hormones to stimulate my ovaries to make eggs. After about ten days of being a human pin cushion, I morphed into a hormone-fueled psycho crazy woman having blood tests and ultrasounds every other day,” Jess says.
“First, I was sedated, and when I woke up, the doctor had removed the eggs. These were then fertilised ex-utero, outside the body, in a container with my husband’s sperm.
“The resulting embryos were then monitored and allowed to develop in a petri dish for five days before being frozen and stored. During this process, a couple (of embryos) die off every day until you only have a few left. I started with 13 and ended up with five. By the way, you have to pay ‘storage fees’ for your little embryos, so you rent a ‘frozen space’ for them to live.
“My husband and I always laugh that when our future children ask where they come from, we will drive past the hospital and point up at ‘Level Three.’”
Note that Jess chose to freeze embryos, whereas women without a partner or with a female partner may decide to freeze just the eggs (oocyte cryopreservation) and organise fertilisation later.
On standby
Dr Rodgers says no matter what your cancer diagnosis is, it’s always valuable to have an appointment with a fertility specialist before any treatment gets underway.
“I always arrange to see the patients within 24 hours. So, if someone rings my rooms or the public hospital and says they need urgent fertility preservation, we’ll work out a way to see them quickly,” Dr Rodgers says.
“There’s no harm in having the conversation, as opposed to coming back to see me after the cancer treatment, and I can’t help at that point because the ovaries have been damaged. So it’s always best to make an appointment as soon as you can, rather than regretting that you didn’t do something about it right away.”
Resources
Further Reading
- Further reading on preserving fertility in females with cancer
Specialists
- Visit the website of Dr Rachel Rodgers
Podcasts
- BNCA podcast on fertility with Sally Obermeder
- Listen to the episode DAHLIA’S STORY… Cancer, IVF, and living with a stoma on the podcast 25 Stay Alive
Webinars
- Pink Hope Australia webinar featuring special guest, Dr Raewyn Teirney on the topic of fertility management for high-risk women
YouTube
We would love to know any resources you found helpful which we can share to help others. Please get in contact.