iCAN
Getting clear on integrative oncology
When it comes to caring for a person with cancer, health experts are focusing more and more on a whole-person approach to treat and support people with cancer.
Referred to as integrative medicine by The Clinical Oncology Society of Australia (COSA), this ‘blending’ of conventional and complementary medicine aims to use the most appropriate, safe and evidence-based care available.
Optimising health
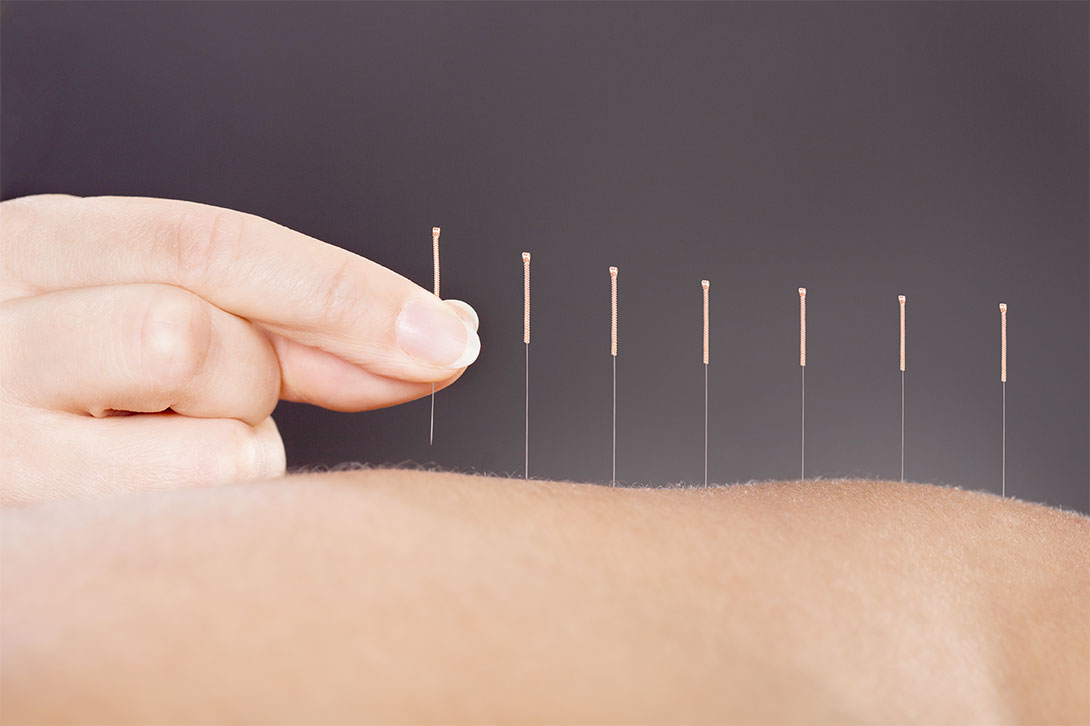
Some cancer centres are adopting integrative oncology, also called integrative medicine, ensuring patients have access to conventional cancer treatments such as chemotherapy as well as evidence-based complementary therapies such as acupuncture and yoga. One such cancer centre is the Chris O’Brien Lifehouse in Sydney.
Head of supportive care and integrative oncology at the Chris O’Brien Lifehouse, Dr Judith Lacey, says patients can now access an ‘expanded toolbox’ of care. Helping to manage the disease and its symptoms, this ‘expanded toolbox’ is designed to improve patients’ quality of life.
“It’s all about looking at what happens to people during the cancer experience,” she says.
“The idea is to develop a personalised approach to optimise a person’s health. We want to improve their quality of life and well-being and find the best ways to help them recover from treatment. Where we can, we also work on preventing cancer recurrence.”
Complementary vs alternative vs integrative
Dr Lacey says that the integrative approach, first coined under the acronym CAM, stands for ‘complementary and alternative medicine’ (as stated in the COSA position statement).
However, the concept of CAM, while laudable as an idea, is problematic in terminology. While complementary therapies refer to those used alongside conventional medicine such as surgery and radiation, alternative therapies, as the name implies, are often touted as replacements for conventional medicine.
The Cancer Council Australia notes that many alternative therapies have not been scientifically tested, and there is no proof they stop cancer from growing or spreading. It also says that once tested; some therapies have proven to be ineffective.
“While side effects of alternative treatments are not always known, some are serious and can delay or stop the cancer being treated effectively,” the Council explains.
According to a 2014 overview of integrative oncology, published in the National Library of Medicine, combining the two terms complementary and alternative confuses the issue. It does a disservice to patients and medical professionals.
“Alternative therapies typically are promoted literally as such; as a replacement for conventional therapies. They lack biological plausibility and scientific evidence of safety and efficacy. Many are outright fraudulent,” the review notes.
“Complementary and integrative modalities have demonstrated safety value and benefits. If the same were true for ‘alternatives, they would not be ‘alternatives’. Rather, they would become part of mainstream cancer care.”
To emphasise its position, the Cancer Council does not recommend using alternative therapies as treatments for cancer. Only the use of complementary therapies that are proven safe and effective is supported.
If your alternative practitioner is not registered with a governing body or professional association or has no accreditation, then these are warning signs.
Above all, patients should steer clear of any practitioner who asks them not to mention their alternative therapy to a treating doctor and specialist.
Alternative therapies cannot take the place of the years of research that mainstream therapies have undergone.
If you are considering an alternative therapy, discuss it thoroughly with your oncologist, cancer care nurse, care team or someone qualified to assess your condition.
Uniting complementary therapies and mainstream oncology
Dr Lacey reports that the term ‘integrative oncology’ is now being used in cancer care in place of CAM.
The 2014 overview of integrative oncology states that combining complementary therapies with mainstream oncology care forms the practice of integrative oncology. The approach is designed to address patients’ physical, psychological and spiritual wellbeing.
“By recommending nonpharmacologic procedures that reduce the impact of symptoms and improve quality of life, doctors can empower patients to play a role in their care. For those impacted by a diagnosis, this approach can also improve the doctor-patient relationship, the quality of cancer care and the well-being of patients and their families,” the report states.
The evidence for an integrative approach with complementary therapies?
As the use of complementary therapies for general health increases, scientific testing is identifying whether they are safe and effective for people with cancer.
Dr Lacey reports that the field is rapidly developing, and evidence is increasing all the time. Some complementary therapies have been found to improve specific symptoms such as fatigue, peripheral neuropathy and nausea. The combination of complementary and conventional therapies also sees an overall increase in well-being.
A 2019 medical review, published in the Journal of Clinical Oncology, made a series of recommendations about the use of integrative oncology in people with breast cancer. It found that acupuncture helped reduce chemotherapy-induced nausea and vomiting, while meditation and yoga improved quality of life and reduced anxiety and stress.
The American Society of Clinical Oncology endorsed the review, which recommended considering acupuncture and yoga for improving post-treatment fatigue.
Another medical review from 2013, published in the US National Library of Medicine, suggests that cancer patients suffering pain might benefit from acupuncture treatment.
Lacey also notes there is also strong evidence supporting exercise during conventional treatment to improve general quality of life.
How do I know what’s safe?
First things first, always start by speaking to your oncologist. Ask them about all the options available to you to help you stay well during conventional treatment.
“In this day and age, there is no reason to look outside of conventional therapy for optimal cancer care. It is really about looking at what other therapies can do to complement your conventional cancer therapy,” Dr Lacey says.
The Cancer Council also encourages patients to discuss any potential or current therapy with their doctors.
“It’s important to tell your doctors before you start using any complementary therapy, especially if you are having chemotherapy, radiation therapy or taking medicines,” the council recommends.
Both the Cancer Council and COSA recommend that health professionals actively seek information from their patients regarding the use of any complementary therapies. They can then discuss the evidence with the patient.
Dr Lacey emphasises that although there is a lot of online information, your doctors should always be your first port of call when considering any sort of complementary or integrative therapy.
Resources
Further reading
- Download cancer.org’s guide to complementary therapies for people with cancer, their family and friends.
- View Society for Integrative Oncology evidence-based guidelines on the use of integrative therapies.
- Read an overview article on integrative oncology at PubMed.gov.
- Read COSA’s position statement on complementary and alternative therapies.
- Read Cancer Australia’s complementary and alternative therapies.
Specialists
- Read more on Associate Professor Judith Lacey.
Podcasts
- Tune in to the You Me & The Big C: The Alternatives podcast.
- Listen to Dr Santosh podcast series on integrative oncology.
Webinars
- View the BCNA webcast on complementary therapies for breast cancer.
YouTube
Associate Professor Judith Lacey on Integrative Oncology
We would love to know any resources you found helpful which we can share to help others. Please get in contact.